Hundreds of thousands of Americans with dementia – and millions around the world – may actually have a very treatable liver condition, a study suggests.
Researchers found that 10 percent of US veterans diagnosed with dementia did not were actually suffering from hepatic encephalopathy (HE) – severe liver scarring which can cause cognitive issues similar to Alzheimer’s.
When damage continues over an extended period of time, the liver cannot detoxify the blood, which allows toxins to build up and reach the brain.
HE can be very mild and difficult to diagnose – for example, not all patients with cirrhosis have it – and symptoms can be as subtle as changes in sleep pattern or irritability.
But once diagnosed, it can be treated with common drugs. This is typically done with laxatives that help to remove ammonia and other toxins that accumulate in the gut, followed by antibiotics which kill some of the harmful ammonia-producing bacteria in the gut.
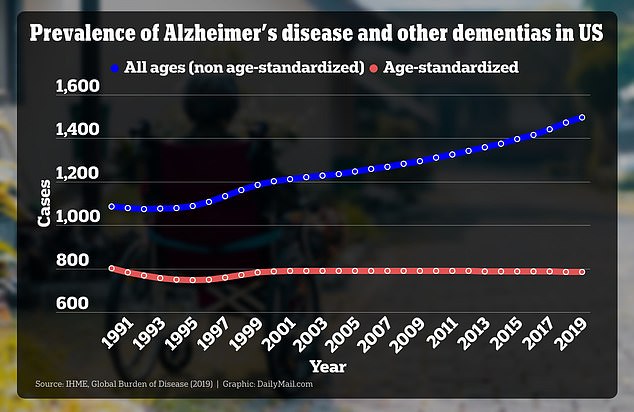
The above graph shows rates of Alzheimer’s per 100,000 people, both age-standardized and all ages. Age-standardization is a method used to adjust for differences in age distribution between populations or over time, while non-age-standardized is the raw rate calculated across all age groups in the population without any adjustment

A recent study of US veterans found that 10% of those diagnosed with dementia actually had a liver condition called hepatic encephalopathy (HE) – a treatable condition
Dementia, on the other hand, is a condition caused by long-term damage to brain cells and function.
In the case of vascular dementia, it’s caused by a lack of blood flow to the brain because of damage to small blood vessels through diabetes or high blood pressure.
Alzheimer’s, the most common form of dementia, is caused when plaques build up in the brain and cause people’s memories and other cognitive abilities to degrade.
While there are some drugs that modestly slow down the progression of dementia, it is incurable.
Dr Jasmohan Bajaj, the lead author of the new study, said: ‘This unexpected link between dementia and liver health emphasizes the importance of screening patients for potentially treatable contributors to cognitive decline.
‘Early detection of liver issues allows for targeted interventions and opens avenues for addressing treatable factors contributing to cognitive decline.’
More than 100 million Americans have some form of liver disease, including around 80 millions with fatty liver disease and don’t know it. Meanwhile, more than eight million Americans have dementia.
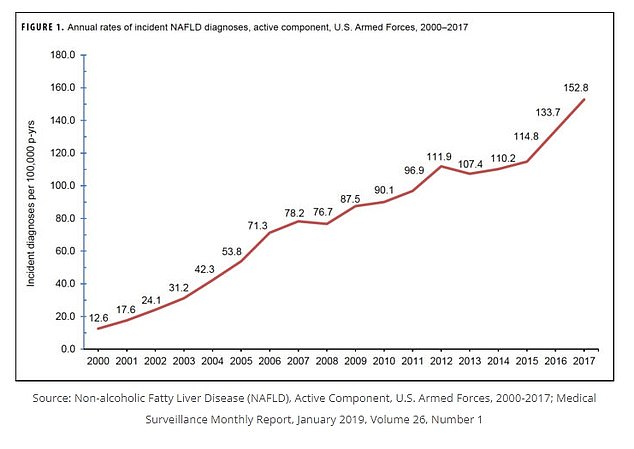
Cases of liver disease have increased over the past two decades, according to a study that looked at rates of the condition among members of the military
In the new study, doctors at the Veterans Health Administration studied more than 177,000 veterans who were diagnosed with dementia over two clinic visits between 2009 and 2019. Roughly 30 percent of them suffered from liver disease.
They looked at the group’s blood results and used them to calculate their Fibrosis-4 (FIB-4) scores, a score based on liver blood results and age, which predicts liver damage.
Over 175,000 people were included in the analysis. Of these, 10 percent had a FIB-4 score of more than 3.25 – the cut-off for the diagnosis of liver scarring.
A high score was less likely in people who had diabetes, high blood pressure or kidney disease – all risk factors for dementia.
But a high FIB-4 score was more common in those with viral hepatitis and heavy alcohol users – both of which are leading risk factors for liver disease.
This suggests that people with a high FIB-4 score may actually have liver disease with HE causing their symptoms rather than dementia, the authors said.
If the liver becomes scarred, it loses its ability to do its job – removing toxins that have a poisoning effect on brain cells.
When this causes HE, a patient is likely to experience a series of changes that mirror those caused by dementia, including cognitive decline and impaired motor skills, as well as poor sleep and mood.
HE occurs in the brains of about 50 percent of people with cirrhosis, which results from the toxic effect that toxins like ammonia and manganese have on brain cells.
Deaths due to cirrhosis are up, and cases have increased over the past two decades, according to a study that looked at rates of the condition among members of the military.
At the same time rates of Alzheimer’s and other dementias have increased steadily since around 2000, and they are expected to keep climbing.
The study had some significant caveats. Ninety-seven percent of the study subjects were male, and 80 percent of them were white, even though most dementia patients are women, Hispanic, or Black.
It also may have relied too heavily on the FIB-4 score, which does not give conclusive evidence of liver disease.
Their study was published in the journal JAMA Network Open.
The liver can be damaged in a variety of ways, including fatty deposits, alcohol use, and viruses – hepatitis is the most common type of liver disease.
When damage continues over an extended period of time, scarring can occur and at a certain point, the liver cannot detoxify the blood. Those toxins can build up and reach the brain, causing HE.
HE can be deadly, though it’s treatable with laxatives to remove ammonia and other toxins that build up in the gut, followed by an antibiotic that kills harmful bacteria.










